Athletes and Blood Clots
 Healthcare providers may delay or miss blood clot diagnoses, including deep vein thrombosis (DVT) and pulmonary embolism (PE), among athletes who exhibit classic symptoms.
Healthcare providers may delay or miss blood clot diagnoses, including deep vein thrombosis (DVT) and pulmonary embolism (PE), among athletes who exhibit classic symptoms.
Why?
Because healthcare providers often don’t consider blood clots as something that affects athletes. Blood clots are uncommon in young, healthy individuals – and most athletes are young and healthy. So, for that reason, DVT, PE, and arterial clots in athletes are not the norm.
To understand how this problem affects athletes, you must first understand blood clot terminology. Your body is composed of an endless tunnel of arteries and veins through which blood flows throughout the body.
Veins carry blood to the heart from the rest of your body. Clots in the deep veins of the legs, arms, pelvis, abdomen, or around the brain are called deep vein thrombosis (DVT). If a piece of the clot breaks off from a leg or arm and travels to the lung, it can cause a clot in the lung, which is called a pulmonary embolism or PE. This can be a life threatening medical emergency. You need to seek immediate medical attention if you have symptoms of a PE.
Arteries are the blood vessels that carry the blood from the heart to other parts of the body, including the brain, internal organs, legs, and arms. Clots in an arteries lead to stroke, heart attack, or limb-threatening peripheral arterial clots, causing a painful, cold, and pale arm or leg.
Symptoms of blood clots in athletes may be misinterpreted as something less serious. Healthcare providers may interpret the leg symptoms from DVTs as a muscle tear, charley horse, twisted ankle, or shin splints. Chest symptoms from PE are often attributed to a pulled muscle, costochondritis (inflammation of the joint between ribs and breast bone), bronchitis, asthma, or a pneumonia.
Athlete-Specific Risk Factors for Clots
Being an apparently healthy athlete does not prevent a person from developing blood clots. Several circumstances put athletes at increased risk for DVT and PE. Athletes, coaches, and trainers should be particularly aware of these risk factors:
- Traveling long distances to and from a sports competition
- Dehydration during and after a strenuous sporting event
- Significant trauma
- Immobilization (brace or cast)
- Bone fracture or major surgery
- Birth control pills, pregnancy, and hormone replacement therapy
- Family history of DVT or PE
- An inherited or acquired clotting disorder (factor V Leiden, prothrombin 20210 mutation, antiphospholipid antibodies, and others)
- A congenital abnormality of the anatomy of the veins, including May-Thurner Syndrome (narrowing of the major left pelvic vein)
- Narrowing or absence of the inferior vena cava (the main vein in the abdomen)
- Cervical rib causing thoracic outlet obstruction
 Time Out: Studies Show Important Trends
Time Out: Studies Show Important Trends
Two studies have evaluated the risk for blood clots associated with marathon or endurance athletes. These studies, conducted by Claire Hull, PhD, and her colleagues in the United Kingdom, appear below.
Hull and Harris (2013)_Circulation (2)
Hull et al. (2014)_Scand J SMS
Go on Offense: Know the Risk Factors for DVT and PE in Athletes
The most common clots occurring in athletes are DVTs of the leg and PE. In addition to the potential risk factors for athletes and non-athletes outlined above, there are a few risk factors that predispose younger people and athletes to DVT and PE:
- Thoracic outlet obstruction or effort thrombosis. In some individuals, an extra rib, excess muscle, or tendon tissue compresses the big vein in the upper chest (subclavian vein) that drains the blood from your arm. This compression typically gets worse when you lift your arm up. This obstruction, often combined with repeated trauma to your vein (from throwing, weight lifting, etc.), may cause a DVT to form in this area, extending into your arm veins. This is called effort thrombosis or thoracic outlet obstruction/syndrome.
- May-Thurner syndrome. This is a congenital anatomic or mechanical variation that predisposes you to DVTs in the left leg. In people with May-Thurner syndrome, DVTs form when the main left pelvic vein is compressed by the overlying main right pelvic artery. This increases the risk of clot formation at the site of this narrowing in the left pelvis. If the DVT resolves, the narrowing can be opened up by a radiologist with a balloon angioplasty and then kept open by placing a stent (or tube) to keep the site open.
- Congenital absence or malformation of the vena cava. Congenital abnormalities of the anatomy of the big vein in the abdomen (vena cava) or pelvic veins can be a cause of DVT in young people. The abnormal anatomy could lead to disturbed blood flow and an increased risk of clotting.
Get Your Head in the Game: Recognize Blood Clot Symptoms
 It’s important to remain vigilant about the signs and symptoms of blood clots. These include:
It’s important to remain vigilant about the signs and symptoms of blood clots. These include:
Deep Vein Thrombosis (DVT)
- Swelling, usually in the leg, but it can also occur in the arm in weightlifters, gymnasts, rowers, etc.
- Leg (or arm) pain or tenderness, usually described as a cramp or charley horse
- Reddish or bluish skin discoloration
- Leg warm to touch
Pulmonary Embolism (PE)
- Sudden shortness of breath
- Chest pain that’s sharp and stabbing; may get worse with deep breath
- Rapid heart rate
- Fainting or passing out
- Unexplained cough, sometimes with bloody mucus
Treatment Considerations
Treatment decisions for people who have blood clots must be individualized. This is particularly true for young, apparently healthy individuals, such as athletes. In the case of unexplained DVT, testing for an inherited or acquired clotting disorder may be appropriate. Read more about blood clot treatment options here.
Defense Wins Games: How to Prevent Blood Clots
- Take breaks and stretch legs when traveling long distances
- Stay well hydrated during and after strenuous sporting events and travel
- Know the symptoms of DVT and PE and seek medical attention if they occur
- Be aware of the risk factors for blood clots
- Find out if your family has a history of blood clots
- In case of major surgery, trauma, prolonged immobility, or when in a cast: ask your doctor about the plan to prevent blood clots.
The Clotting Process
 The body is designed to balance the factors in the blood that cause clots and the factors that dissolve them.
The body is designed to balance the factors in the blood that cause clots and the factors that dissolve them.
Blood clots can occur when:
- There is an imbalance between the two systems that keep the clotting process in your blood in check. There could be too much activity of the proteins and platelets that form clots (the procoagulant system), or too little activity of the fibrinolytic system, which dissolves blood clots as they form.
- You have trauma to a blood vessel, including a bone fracture or thoracic outlet obstruction as defined above.
- Your blood flow from your arms and legs to your heart is impaired from sitting with your legs bent for a prolonged period of time.
- Your blood is “thicker” than usual, which occurs during dehydration, using the drug erythropoietin (EPO), or receiving excessive blood transfusions.
Unfortunately, few studies exist that investigate the connection between physical activity and blood clot formation. So, we don’t know the exact net effect of training on this clotting balance mechanism.
However, we do know that blood levels of the clotting protein factor VIII increase with exercise and that the elevation persists during recovery. This could lead to an increased risk of blood clots in athletes. But data also indicate that the fibrinolytic system that dissolves blood clots is overactive in people who exercise.
Psychosocial Implications
After a DVT or PE, athletes can experience a decline in physical functioning, also called deconditioning. Depression can also set in after such a life-changing event. Patient support groups, such as Team Stop The Clot Facebook Group, may be helpful in this situation, as may antidepressants.
Selected references for the above article:
- El-Sayed MS et al: Exercise and training effects on blood haemostasis in health and disease: an update. Sports Med 2004;34(3):181-200.
- Shrier I, Kahn SR: Effect of physical activity after recent deep venous thrombosis: a cohort study. Medicine and Science in Sports and Exercise 2005;37: 630-634.
- Roberts WO, Christie DM: Return to training and competition after deep venous calf thrombosis. Medicine and Science in Sports and Exercise 1992;24:2
Additional Resources for Athletes
- NBCA Sports and Wellness Institute. It is our goal to provide athletes of all levels with a strong support system to help them bounce back and ultimately thrive following a blood clotting event. We are here to help. You have what it takes to join the team, and you can skip the try-outs! This is a team where everyone gets to play, no matter what their experience level may be. Join us today.
- Clot Buster. Our friend Roland Varga has a blog that follows athletes return to their sport after blood clots.
- Venous thrombosis in athletes. (2013) Article from the Journal of the American Academy of Orthopaedic Surgeons. (Abstract only) Authors: Grabowski G, Whiteside WK, Kanwisher M.
- Skater Tara Lipinski Speaks Out About DVT (2011) from NIH Medline Plus National Institutes of Health
- Venous Thromboembolism and Marathon Athletes (2013) A patient oriented article that discusses why athletes are at risk of blood clots, signs and symptoms of blood clots, and advice to returning athletes From the American Heart Associations’ Circulation Journal
- Hypercoagulability in athletes (2004) Article from Current Sports Medicine Reports. Discusses the conditions athletes face that can result in exposure to several risk factors for blood clots, how to address the risks, prevent blood clots and return to sport. (Abstract only) Authors: Meyering C, Howard T.
- Thromboembolic disorders: guidance for return-to-play (2011) Article from Current Sports Medicine Reports. Discusses VTE recovery and the structured step by step return-to-training program with progressive increase in intensity for the road back to play for athletes. (Abstract only) Author: Depenbrock PJ.
- Deep Vein Thrombosis in Athletes: Risks of Racing and Resting (2010) Article from the American Medical Athletic Association Journal that discusses how blood clots form, the impact of exercise on the clotting process, misdiagnosis of blood clots in athletes, and blood clot risks common to athletes.
- Blood Clots and the Athlete: A Review of Deep Vein Thrombosis in Sports (2007) Article discusses the formation of blood clots, prevention of blood clots, risk factors including thrombophilias or hypercoagulability disorders, and return-to-play issues. From American Medical Society for Sports Medicine’s Athletic Therapy Today.
- Deep Vein Thrombosis in Athletes: Prevention and Treatment (2012) A chapter from a book “Sports Injuries” that discusses the risk factors, diagnosis, prevention, and treatment of DVT and PE in athletes. (Abstract only) Authors: Faik Altıntaş, Çağatay Uluçay.
- How To Prevent Blood Clots After Destination Races (2013) Useful tips from Women’s Running to prevent blood clots after the race when you are at risk during travel. Read the National Blood Clot Alliance’s blood clot travel safety tips
- Runners and Blood Clots: What You Need to Know (2013) Useful tips from Runner’s World on the risks of blood clots for runners, what signs and symptoms of clots to look for, and strategies for prevention of blood clots.
- Athletes and Anticoagulation: Return to Play After DVT/PE (2016) Article from The American College of Cardiology discusses whether or not athletes need to be prevented from competing in contact sports while being anticoagulated. Authors: Josh Berkowitz, MD; Stephan Moll, MD
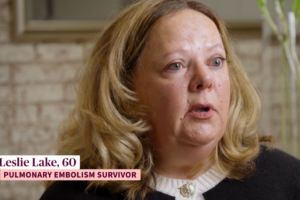
Read Stories of Athletes who have had Blood Clots
- Eric O’Connor, Blood Clot Survivor, Marathon Runner, and Past NBCA Board President
- Tim Allen Tells His Blood Clot Survival Story
- In Memory of Kyle Baca: His Blood Clot Story as Told by His Mother
- Rebekah Bradford’s Blood Clot Story
- Dan Capobianco Tells His Blood Clot Survival Story
- Jim Fenton’s Blood Clot Survival Story
- Hope’s Story of Blood Clots as a Warning Sign for Cancer
- Michelle Winters’ Blood Clot Story