Blood Clot FAQs – Deep Vein Thrombosis (DVT) and Pulmonary Embolism Follow Up Care
What is the likelihood of developing another deep vein thrombosis (DVT or blood clot in the leg)?
A person who had a DVT is at higher risk to develop another one than someone who never had one. The degree of increased risk depends upon individual medical history, and includes factors such as family history of a blood clot, location of the clot, whether there was a previous clot or a clotting disorder, and certain “triggers.” Notable “triggers” are hospitalization for more than 3 days, surgery, knee or hip replacement, and trauma.
What are the signs and symptoms of a DVT?
- Swelling, usually in one leg
- Leg pain or tenderness
- Reddish or bluish skin discoloration
- Leg warm to touch
Make an appointment to see your doctor if you think you might have a DVT, and let him or her know your symptoms.
Will my swelling and go away?
It is common for swelling to remain in the leg for awhile. Your compression stockings help increase blood flow in your legs to reduce swelling and to prevent any complications from the DVT.
What are the warning signs of a pulmonary embolism (PE or blood clot in the lung)?
- Sudden shortness of breath
- Chest pain that is sharp or stabbing and may get worse with each breath
- Rapid heart rate
- Unexplained cough, sometimes with bloody mucus
- A PE is a medical emergency and you should seek medical attention right away!
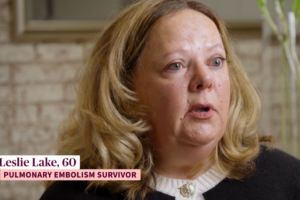
What should I expect after a pulmonary embolism (PE)?
Shortness of breath and mild pain or pressure in the lungs are common. You are likely to notice pain when you exert yourself or during physical activity or whenever you take a deep breath. Shortness of breath gets better in time, and exercise helps you use your breath more efficiently.
Whom should I tell that I am taking blood thinners?
Tell all of your doctors, nurses, dentist, or healthcare providers.
Taking Coumadin® (warfarin) helped me feel safe from having another clot. Now that I don’t have to continue blood thinners, I feel uneasy.
This is a common feeling, and you should discuss your feeling of uneasiness with your doctor. The most worrisome side effect is bleeding, but if you take your blood thinner and follow your INR level as directed, you and your doctor can make taking an oral blood thinner as safe as possible.
If I'm ever hospitalized, should I tell the doctors that I had a DVT or PE?
Absolutely. Tell this to any doctor or healthcare professional who takes care of you, in or out of the hospital.
Is it OK to exercise?
The amount and type of exercise that is safe is a decision to make with your doctor, and depends on your physical condition. Walking or swimming are usually considered good choices as exercise.
How helpful is exercise after a DVT or PE?
Exercise increases circulation, reduces swelling, and helps you feel invigorated. Aerobic exercise may increase lung function after a PE.
Is crossing my legs a problem after a DVT?
Crossing your legs limits free flow of blood through your legs. Good circulation is important to prevent clots.
How long should I sit at one time?
You should do heel toe exercises and circle your feet whenever you are sitting. Try to get up and walk around at least every 2 hours.
Is it OK to travel after having a blood clot?
Yes. Stop every hour, get out of your car, and walk for several minutes. If you are on a plane, train, or bus, try to sit where you can stretch your legs (aisle seat, exit aisle). Get up and walk the aisle(s) whenever it is safe. If you cannot get out into the aisle, do heel toe exercises and foot circles while seated to keep your blood flowing. It is also a good idea to wear compression stockings consistently if you have had a DVT, and this includes while traveling. Wear loose fitted clothing, and drink a lot of water. Sometimes your doctor will suggest a dose of a low molecular weight heparin prior to lengthy travel.