Total Knee Replacement Patient Story
Avoiding a Blood Clot After Total Knee Replacement Surgery: A Patient Story
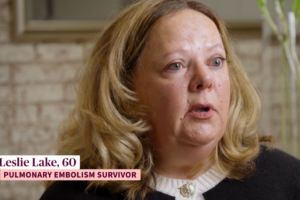
My story is a little different from most total knee replacement (TKR) patients, but the lessons I learned pre and post-op will help anyone avoid blood clots.
I have a clotting disorder (protein C deficiency), which makes me an “Uber Clotter,” that was discovered several years ago when I had major clots in both of my lungs or pulmonary emboli (PE). It was the perfect storm that led to the discovery of my disorder was an arthroscopic knee surgery, birth control, and a cross-country flight. Any of those can cause blood clots, but add my disorder to the mix and that story ends with me getting off a flight unable to breathe and being rushed to an ER. I was a very active person in my forties.
So I went into my TKR as a patient who takes warfarin daily with the same fears everyone has undertaking a major surgery. I did a lot of pre-op online research, but I will tell you that unless information is coming from an organization like the Agency for Healthcare Research and Quality, or NBCA, you are going to find a lot of personal stories online that will most likely scare you. And don’t watch the Youtube videos unless you are a person who needs TMI.
What will help you is a plan, similar to the one I had.
Talk to your doctor and make sure your questions are answered.
Discuss your risks, and what you can do to lessen them. Blood clots are a risk with any type of surgery, and for people with limited mobility, so be sure to ask a lot of questions or take someone with you who can write instructions down. Click here are several great questions to ask your doctor.
Your doctor will have a plan and recommendations for you, knowing your current medications and history. Prevention is typically a three-pronged approach designed to address the issues of stasis (or inactivity) and coagulation. Typically several therapies are used in combination. For example, you may be fitted with graded compression elastic stockings and an external compression device upon admittance to the hospital. Movement and rehabilitation begin the first day after surgery and can continue for several months and anticoagulant therapy may begin the night before surgery and continue after you are discharged.
Exercise prior to surgery.
You are most likely having the surery because you are in pain, and therefore limited in the amount of exercise you are able to do. It is, however, truly important that you go into the surgery as aerobically fit as you can be, and with as much muscle as you can develop.
Click here for a video that will give you some aerobic training, without moving your legs.
Click here for another that will help you with upper body strength.
It is important that you do not try any new exercise without first consulting your doctor.
Attend a pre-op program many hospitals sponsor.
My hospital had a pre-op training session with a nurse for hip and knee replacement surgery patients. If you can, take someone with you as it never hurts to have a second set of ears. Ask questions about what therapies the hospital uses to decrease the likelihood of clots during your stay there.
Once you are post-surgery, get moving.
Believe it or not you will be standing and walking using an assisted device during the first 24 hours after surgery. The more active you are, the less likely you will clot. Do what the nurses tell you to.
Click here for an example of how much activity you will be expected to perform post-op.
Develop an exercise regime with your physical therapist, and walk as much as you can tolerate.
This will help you heal and keep your blood flowing. It is very important to exercise, take your medicine as your doctor prescribes, or use the compression stockings during this time when you are healing. Enlist family and friends to help you with walks and exercises—you might need the additional motivation, and its best to walk with someone.
Click here for an example of the exercises you will be doing with your physical therapist.
Know the symptoms of a blood clot.
After knee surgery, most DVTs occur in the calf. Although less likely to lead to PE, these clots are more difficult to detect. Less than one third of patients with DVT present with the classic signs of calf discomfort, edema, distended veins, or foot pain.
The risk of developing DVT extends for at least three months after TKR. The risk is greatest two to five days after surgery; and a second peak development period occurs about 10 days after surgery, so be aware.
You will be on pain medication, and your knee will be swollen. Call your doctor if you experience any symptoms of blood clots including shortness of breath, as this could be a sign of a life-threatening PE, cramping in your calf, or pain in your foot or ankle.