In June 2011, 16 weeks after giving birth to my first child, I started having symptoms of back pain. As a 23-year-old new mother, I diagnosed myself with all sorts of things. I decided that the pain I was experiencing must be my kidneys reacting to alcohol after such a long time without any, and then I thought it was sciatica pain in my lower back. After 10 days of kidding myself, I undressed and was unable to remove my skinny jeans, because my leg was swollen. It was also discolored, and after a few minutes on the phone with National Health Service Direct – the United Kingdom’s health information line – it was clear I needed to go to the hospital. I drove myself and my 16-week-old daughter to the hospital, where I was instantly given heparin blood thinners and a scan. My DVT was huge, and it was located between my groin and belly button. After a hysterical night in the hospital spent separated from my baby, I was discharged on the oral anticoagulant warfarin.
A week later, I was back in hospital because my symptoms got worse. I was scanned again by the same sonographer I had seen a week earlier. She said, “Last week your clot was huge, now it’s ginormous.” I was taken back into hospital and an IVC filter was inserted into my vein to stop the clot from traveling to my lungs. The filter was removed approximately four months later, when the clot had hardened and was not at risk of traveling through my blood stream. After that, I had an increased INR target, and lived life on warfarin for two years.
During those two years, my husband and I discussed with numerous professionals how we might be able to have another baby. Three years after the birth of our daughter, we welcomed our lovely son. It wasn’t easy. I injected blood thinners daily for the entire time we were trying to conceive, during pregnancy, and for six weeks after the birth of our son. I went to a hospital an hour drive away from me every two weeks for checks, and was then induced, giving birth while managing clotting and bleeding risks.
After settling back into life on warfarin, I decided that it wasn’t for me. It was just too high maintenance for someone like me, who was 26 years old, with a full-time job, and two small children. I started to research alternatives and found out about the new oral anticoagulants, and thankfully my specialist agreed it would be a good move for me to switch to it. The new oral anticoagulant I am taking changed my life. I saw my doctor every six months, and life was good. Thank God for the National Health Service!
My next issue was post-thrombotic syndrome. I managed the best I could. I could walk and even jog a little bit, but after a long day, I was in pain. My leg throbbed and the constant feeling of pulling a ball and chain started wearing me down. The turning point for me was a day trip to London in September 2016. A boozy, sightseeing day with the girls turned bad for me when I couldn’t keep up. At 29 years old, I felt very sorry for myself. Have you ever tried to get off a tube, or underground transport, escalator when you can’t lift one of your legs? I hope not, because it’s near impossible and very humiliating.
I started discussing solutions for my post-thrombotic syndrome with my doctor in Manchester, England. He happily referred me to an equally wonderful specialist, based in Nottingham, England, who is well known for helping people with problems like mine. Just before Easter 2017, I went to see him. It was a two-hour drive to get there. My friend came with me, and we made a day of it. The clinic I went to was amazing, and I was able to get everything I needed there. I had an ultrasound on my veins, blood tests, and a visit with my new specialist. I learned that my veins were as horrendous as I expected, and the specialist explained what I already suspected. I had May-Thurner Syndrome, and in essence, my artery had collapsed on top of my vein in my pelvis area, probably following the trauma to the area from my pregnancy. I was sad about how awful the ultrasound results were, but hopeful there would be a solution. I scheduled a procedure to stent my veins, as my specialist was confident we could work it all out.
In May 2017, I went back to the clinic in Nottingham. On the first day, I had another ultrasound, CT scan, and the usual pre-op checks. I cried all day. It was my first-ever operation, and the first time I would be away from the children for two days. I had been to my general practitioner, who gave me anti-anxiety medication to get me through the experience.
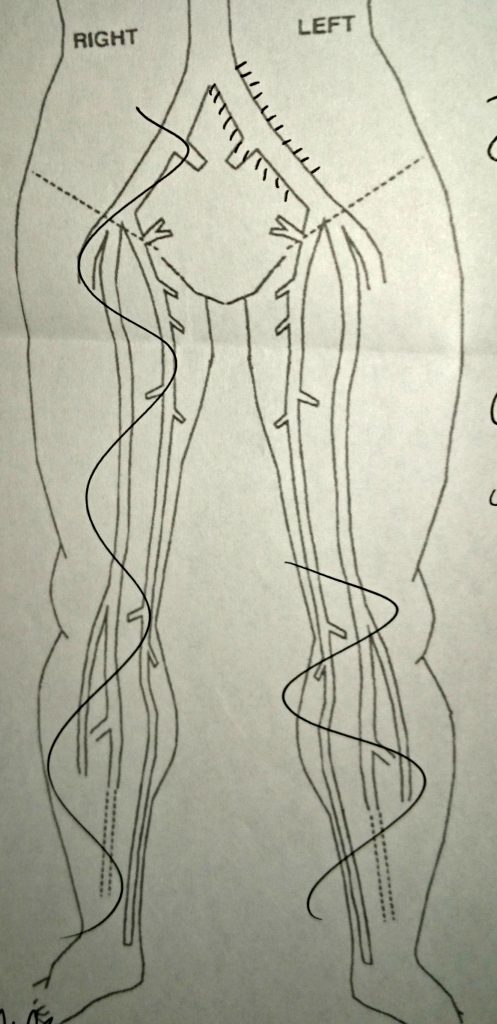 The second day, I went to hospital and was put under a general anesthetic. Two surgeons worked on me, one through an opening of my vein in my neck, and the other through an opening at the top of my leg. They both drilled until they met in the middle, and then put stents through the area to keep the veins open. It wasn’t a pleasant experience, and I was in a fog for around a week after, but I felt instantly better. Now, if you have post-thrombotic syndrome, you will know that lying in bed creates a dull aching pain for some people. I had nothing. I didn’t feel any pain at all in my leg.
The second day, I went to hospital and was put under a general anesthetic. Two surgeons worked on me, one through an opening of my vein in my neck, and the other through an opening at the top of my leg. They both drilled until they met in the middle, and then put stents through the area to keep the veins open. It wasn’t a pleasant experience, and I was in a fog for around a week after, but I felt instantly better. Now, if you have post-thrombotic syndrome, you will know that lying in bed creates a dull aching pain for some people. I had nothing. I didn’t feel any pain at all in my leg.
For two months after the procedure, I could not believe the difference. I wasn’t very brave, because I thought the relief was all in my head. I went back to Nottingham in September 2017 and had another ultrasound scan on my leg. There was nothing there. Nothing at all. Just wonderful, open veins with blood flowing through them. I don’t know when I last felt happiness like that. I was discharged from care at the clinic and off I went, now 30 years old, and back to life without a DVT.
I hope you have found my story useful. If you have a residual DVT and you suffer from any pain, I urge you to speak to your doctors about what opportunities exist to help you. The specialist I saw in Nottingham and the treatment I received there, changed my life.




