What is antiphospholipid antibody syndrome?
Antiphospholipid antibody syndrome is a condition in which the body produces antibodies that target phospholipids (antiphospholipid antibodies). Phospholipids are the molecules that form the membranes of cells, including the cells that make up the endothelium, the smooth slippery surface that lines blood vessels. Antibodies are proteins produced by the body as part of its defense mechanism against foreign invaders such as infections. In the case of antiphospholipid syndrome, the antibodies attack phospholipids and damage the endothelium. (See Question 3.)
Individuals who produce such antibodies are at a high risk of developing blood clots in both arteries and veins. Pregnant women who have these antibodies are not only at increased risk of forming blood clots, but—because these antibodies may attack the endothelium of the blood vessels that supply the circulation to the uterus, placenta, and unborn baby—are at increased risk of miscarriage and other pregnancy complications. Other potential pregnancy complications include babies with poor growth (fetal growth restriction), premature separation of the placenta from the uterus (placental abruption), preeclampsia (high blood pressure of pregnancy), and stillbirth.
Several types of phospholipids exist, and different antibodies may be formed against the various types of phospholipids as part of antiphospholipid syndrome. Three antibodies have been shown to be associated with blood clots, miscarriage, and other pregnancy complications: anticardiolipin antibodies, anti-beta2 glycoprotein I antibodies, and the lupus anticoagulant. The lupus anticoagulant is actually misnamed. First, most patients with lupus anticoagulants do not actually have lupus. This antibody was first described in a patient with lupus, which explains that part of the name. Second, the lupus anticoagulant is not an anticoagulant at all. As is true of anticardiolipin antibodies and anti-beta2 glycoprotein I antibodies, individuals who have the lupus anticoagulant are actually at an increased risk of forming blood clots.
The term “lupus anticoagulant” comes from the behavior of plasma taken from individuals with these antibodies during a partial thromboplastin time (aPTT) test. (See Question 21.) The aPTT measures the length of time (in seconds) that it takes for clotting to occur when certain substances are added to the liquid portion of blood in a test tube (plasma). One of these substances is phospholipid. The aPTT test is prolonged when there is a deficiency of certain clotting factors or when heparin is present—two conditions that carry an increased risk for bleeding. In contrast, when the aPTT is prolonged due to interference from antibodies to phospholipids, the patient actually has an increased risk for thrombosis. The lupus anticoagulant is one of the antibodies that binds to phospholipids in this way and frequently causes the aPTT to be prolonged. While the aPTT is used to detect clotting factor deficiencies and to monitor heparin levels, it can also be used to identify antiphospholipid syndrome.
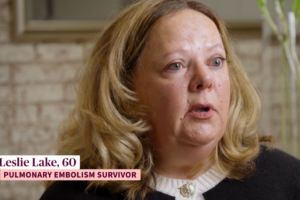
Jennifer’s story:
Four years after I had the blood clot in the vein in my brain, which occurred after I had preeclampsia and had given birth to our daughter, we moved from upstate New York to North Carolina. My hematologist from upstate New York referred me to a university medical center in North Carolina where there was a hematologist who specialized in blood clotting disorders. He monitored my Coumadin® and did blood tests periodically. He told me I have antibodies in my blood that can make me more susceptible to blood clots and verified that I have antiphospholipid syndrome.